PHEM
Pre-Hospital Emergency Medicine (PHEM)
While immediate medical care in one form or another has existed for many hundreds if not thousands of years, more recent history in the UK has seen immediate care provided by motivated volunteers. Over the last few decades the scope and spread of immediate care has evolved significantly.
Increasing opinion that formal training and speciality accreditation was desirable led to Pre-Hospital Emergency Medicine (PHEM) coming into being as an accredited sub-speciality training option in 2011. Since 2013, it has been recognised as a sub-speciality of Anaesthetics, Emergency Medicine and Intensive Care Medicine. Training is the responsibility of The Intercollegiate Board for Training in Pre-Hospital Emergency Medicine (IBTPHEM).

What exactly is it?
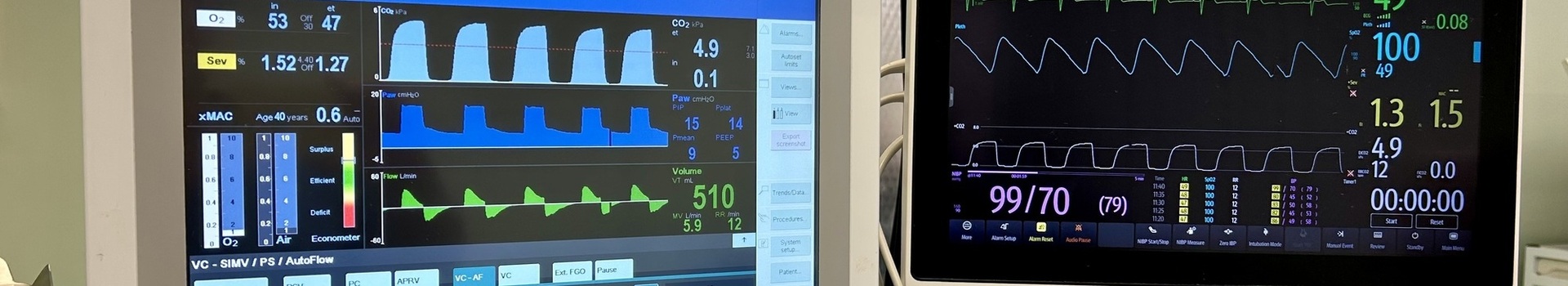
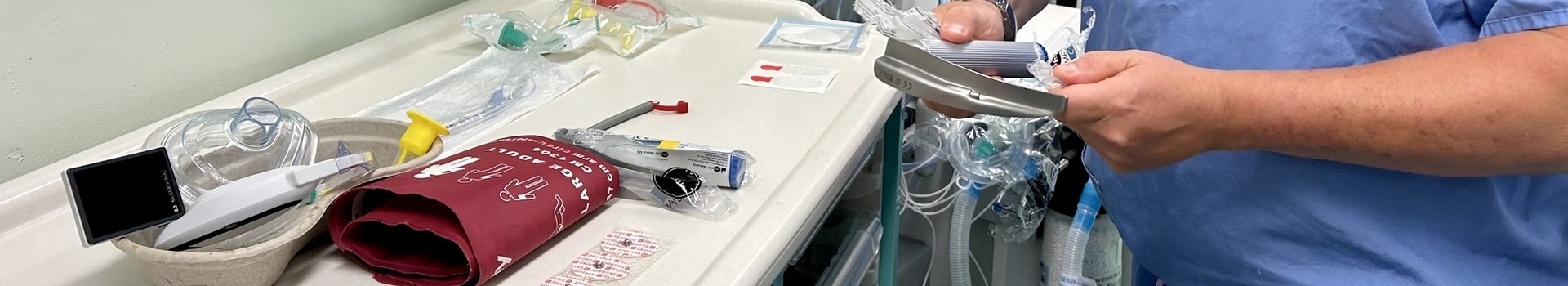
PHEM involves provision of enhanced and critical care for seriously ill or injured patients before they reach hospital (on-scene) or during emergency transfer to or between hospitals (in-transit) in what is often a resource limited and both physically and psychologically challenging setting.
Sub-specialist PHEM practice relates to the Emergency Response, Primary Scene Transfer and Secondary Emergency Transfer at the level of the Consultant (Level 8) practitioner. It represents a unique area of medical practice which requires the focused application of a defined range of knowledge and skills to a level not normally available outside hospital.
Who can apply?
Trainees in Anaesthesia, Emergency Medicine & Intensive Care Medicine with a successful ST5 ARCP who meet the person specification and have the support of their Head of School (HoS) and Training Program Director (TPD).
Since 2021 applications require: “Minimum 6 months training in each of Anaesthesia, Emergency Medicine, Intensive Care Medicine and Acute Internal Medicine in posts approved for training at or above CT1 level or equivalent by intended start date. This will be an 'essential' requirement and applications will need to ensure they meet this in order for their application to be considered.
The recommendation therefore is that aspiring trainees complete ACCS core training. If they have not completed ACCS training, they should discuss their requirements to fulfil the additional EM and Acute Medicine training as OOPE with the TPD as soon as possible. Any qualifying OOPE must be in a post recognised for training.
When can you apply?
Requirement exists for a successful ST5 ARCP is to permit trainees to commence their post, therefore the earliest you can apply is in the beginning of your ST5 year. I would strongly advocate that completion of the Final FRCA examinations should also be considered as a higher priority than applying for PHEM training, if this had not been completed at the end of ST4. Indeed, it would seem unlikely that you would obtain the required HoS/TPD support required to apply prior to this being achieved.
Adverts normally appear on the HEE website in September with applications opening a few weeks later, closing within a few weeks and successfully shortlisted candidates are invited to a selection centre in November. Final offers are then made by December.

Where can you do it?
There are training locations throughout the UK. Over the last few years trainees from Wales across the parent specialities have taken posts in Wales, West Midlands and the South West. The nature of the training means training is typically delivered by an Air Ambulance service, although the IBTPHEM curriculum covers the full spectrum of PHEM practice.
You should try to speak to PHEM trainees who have completed training within deaneries you are keen to work in and bear in mind that you may have to move away to complete your training.
How does the training work?
The extensive curriculum covers 6 domains of PHEM with a number of cross-cutting themes. The training begins with a week long national induction course (the best NHS induction you will ever do!) and local formative assessments culminating in NSA1 at 6 months (the Diploma in Immediate Medical Care) and NSA 2 (Fellowship in Immediate Medical Care) in the last month of training.
In terms of workplace based assessments the recently updated 2022 curriculum now “only” requires 2 MSF and 20 OSAT - many fewer than the 15 CEX, 30 CBD, 10 SIM, 30 DOPS, 2 MSF, 25 ACAT and 5 TO previously required! Fortunately, there is ample provision for supervision and WPBA completion during the 12months of training. An e-portfolio solution, PHEMnet has been developed and since 2018 onwards has been used as the sole method of submission of evidence to the TAP (training assessment panel – a bit like an ARCP) at the end of the training program.
The year is based around full time working in the Pre-Hospital environment, generally delivered between a mix of HEMS and Land based Critical Care team deployments. As trainee experience and competence increases, the amount of direct supervision can decrease to allow “solo” deployment – typically as part of a team with remote “top cover” support.
"The Job"
As a PHEM trainee you will see and so things you could never entertain within your hospital practice. Working often in dangerous, cold, wet and unpleasant environments you will be treating patients of all ages - it will be a challenge, and it will be hard physically and emotionally. It will also be once of the most rewarding experiences of your career. Find a current or completed PHEM trainee and chat to them to find out more about the day to day realities, and if possible speak to someone who has completed training in each of the services to which you intend to apply.
Training in Wales
HIEW hosts training places for one Scheme C (full time over 12 months) and two Scheme A (blended with parent specialty of Emergency Medicine over 24 months) trainees. As such recruitment alternates between 1 and 3 new trainees starting programs biannually in August. Emergency Medicine Training posts are hosted by the All Wales School of Emergency Medicine at The Grange Hospital, Cwmbran.
PHEM Trainees in Wales are employed through Swansea Bay UHB and work within the unique Welsh system, primarily within the Emergency Medical Retrieval and Transfer Service (EMRTS).
This NHS commissioned service operates in partnership with the Wales Air Ambulance Charity with the mission of providing advanced decision-making and critical care for life or limb-threatening emergencies that require transfer for time-critical treatment at an appropriate facility.
Trainees will work across all the EMRTS bases within Wales (North and South) gaining experience of “whole system” pre-hospital critical care practice. Trainees also benefit from close partnerships with the Welsh Ambulance Service, the Adult Critical Care Transfer Service (ACCTS Cymru), regional Community Emergency Medicine Programs and other emergency response agencies to gain exposure to the full breadth of PHEM practice.
During a 12-month full time training program, trainees can expect to undertake a month of Phase 1a which includes attendance at the national induction course as well as local induction training before completing 5 months Phase 1b training with a high degree of consultant supervision. Following successful completion of a local Phase 1 summative “sign off” assessment, trainees are then able to deliver full pre-hospital critical care with remote consultant supervision and will lead the EMRTS duty teams by day and night providing full pre-hospital critical care with remote supervision throughout Phase 2.
PHEM training within Wales offers a unique opportunity to experience a blend of rural and urban PHEM practice within a national NHS system delivering world class care to the people of Wales.
Advice to aspirant PHEM trainees
PHEM training has become incredibly popular, as such it has become incredibly competitive. This is great for the speciality, as it can select the best candidates, but can be very frustrating if you work to apply and don’t get shortlisted.
So how do you make sure you get shortlisted when you apply? Well, firstly work out what you are going to need to have done before you even apply. National recruitment to PHEM is currently hosted by Health Education East of England and you should review the current person specification and recruitment timelines on their website well in advance of your application.
By ‘well in advance’ I mean at minimum 2 years before you are due to apply, as unless you already meet all the essential and desirable criteria; it is likely to take you this long to put in the many, many hours of work required to do this. Given the increasing visibility and popularity of PHEM, the CT1 year during ACCS training is the best good point to start planning your route to application! Remember the aim of producing the best application you can is to get you to the selection centre, on the day at the selection centre its everybody’s job to lose.
Speak to current and recent trainees about the job and how they went about securing a post, if possible try and get a current PHEM practitioner or recent trainee to mentor you and help guide you in the years and months before you apply.
Get involved in PHEM at a basic level. Arrange Foundation Year tasters in PHEM, do ACCS rather than Core Anaesthesia, try to include some PHEM in that year out you are planning after Core Training – maybe even consider planning a year out in a PHEM fellowship.
Arrange some observer shifts with the Ambulance service or a Community Emergency Medicine service such as run in the Grange University Hospital or University Hospital of Wales. Attend your local Air Ambulance Clinical Governance days (EMRTS Cymru run these regularly in Wales) if you are eligible to do so. What ever you manage to do – log it and generate some reflections, it all builds up evidence of your suitability to apply.
The mandatory life support courses listed in the person specification offer opportunities to be selected to instruct. Be open with your mentors on these courses about your desire to achieve IP status, and your motivations for doing so: plan when you will revalidate these courses, remember they need to be in date when you apply for (and start) PHEM training. Also, consider the more difficult to evidence areas of the person specification, things like personal skills and training in Team Resource Management may be best evidenced by a niche course, study day or self-directed learning.
There are several excellent annual conferences (e.g. Trauma Care, Retrieval & the BASICS/FPHC Conference) that offer the opportunity to meet the PHEM community across the UK, and also provide excellent forums to display posters or present on PHEM related scholarly activity. Again, your regional air ambulance or mentor may be able to help with this or you can apply to join the Pre-Hospital Trainee Operated Research Network (PHOTON) to support this aspect of your development.
It feels hard to get a PHEM training job as an anaesthetist. The nature of funding streams for many of the scheme A/B jobs currently means that only emergency physicians can apply which leads to steep competition for those jobs that those from other base specialities are able to apply for. You need to make sure that you work to produce the best application you can, shortlisting for interview has to be your first target. While you are doing this you should also be producing a PHEM portfolio that is well structured, neat and can be used to evidence everything you put on your electronic application.
Think about how far you are able and prepared to move for a job and bear in mind that may mean committing to two years in a different location for a blended job – this will impact on the jobs you can potentially apply for.
Finally, keep fit, stay keen and be enthusiastic about PHEM and one day you may well be fortunate enough to be able to stop describing yourself as “an aspirant PHEM trainee”.
Matt Creed (Consultant in Anaesthetics & Pre-Hospital Emergency Medicine and Deputy TPD for PHEM, University Hospital of Wales)
Matthew.Creed@wales.nhs,uk
September 2023
Points of contact
Wales PHEM TPD Dr Laura Owen Laura.owen@wales.nhs.uk
- EMRTS Cymru https://www.emrts.cymru/
- BASICS Wales is the umbrella organisation that links the following charity organisations:
- MEDSERVE Wales (South Wales BASICS Scheme) https://www.medservewales.org/
- MEDS (Mid Wales BASICS Scheme) http://emergencydoctors.org.uk/
- NWEDS (North Wales BASICS Scheme) https://www.nweds.org.uk/
Welsh Ambulance Service NHS Trust: Dr Jonathan Whelan (Consultant in Anaesthesia & PHEM, Assistant Medical Director WAST) jonathan.whelan2@wales.nhs.uk [Note observer shifts are best arranged for ST3+ aspirant PHEM trainees]